Duodenal Switch
INTRODUCTION
The Duodenal Switch procedure (also called vertical gastrectomy with duodenal switch, biliopancreatic diversion with duodenal switch, DS or BPD-DS) generates weight loss by restricting the amount of food that can be eaten (removal of stomach or vertical gastrectomy) and by limiting the amount of food that is absorbed into the body (intestinal bypass or duodenal switch). It is more controversial because it has a significant component of malabsorption (bypass of the intestinal tract), which seems to augment and help maintain long-term weight loss. Of the procedures that are currently performed for the treatment of obesity, it seems to be the most powerful and effective, but may also have more complications associated with it..
PREPARATION TO THE PROCEDURE
When you are well informed and choose to have a Duodenal Switch then the following investigations have to take place:
1. Laboratory / Blood tests 2. Ultrasound of your abdomen 3. Electrocardiogram with cardiac check-up 4. Chest X-ray with pulmonary check-up 5. Gastroscopy 6. Consultation dietician
In case of regular medication usage one has to inform their surgeon, especially in case of blood thinners (aspirin, anti coagulants, anti-inflammatory drugs, http://www.ncpainmanagement.com/BloodThinners.htm ) as these need to be stopped before surgery.
On the day of surgery you will have to remain sober. If necessary some medication can be taken with a little water.
PROCEDURE
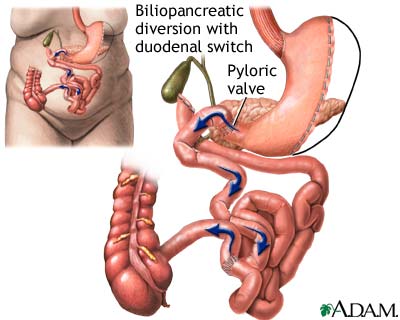
The first part of the procedure is like a Sleeve Gastrectomy. The stomach is restricted by dividing it vertically and removing more than 85% of it. This part of the procedure is not reversible. The stomach that remains is shaped like a banana and measures from 4-7 ounces (120-250cc) depending on the surgeon performing the procedure. The nerves to the stomach and the outlet valve (pylorus) remain intact with the idea of preserving the functions of the stomach while reduing the volume. By comparison, in a Roux-en-Y gastric bypass, the stomach is divided, not removed, and the pylorus is excluded. The Roux-en-Y gastric bypass stomach can be reconnected(reversed) if necessary.
The intestines are divided and rearranged to separate food from the digestive juices, thereby creating malabsorption. The food limb is attached to the duodenum and receives food from the stomach. This limb is 150 cm long. The digestive juices are now separated from the food and travel for over 500 cm in the bypassed small intestine. Both food and digestive juices mix together and travel together for 100 cm in the common limb. Thus, food and digestive juices are separated for most of the length of the intestines. This prevents you from absorbing all of the calories that you eat. By comparison, the intestinal bypass in a Roux-en-Y gastric bypass is much less extensive, and the common limb for digestive juices and food to mix is approximately 5 times longer. Therefore, the Roux-en-Y gastric bypass has minimal malabsorption compared to the Duodenal Switch procedure.
This procedure is completely done by laparoscopy.
SURGERY THROUGH LAPAROSCOPIE
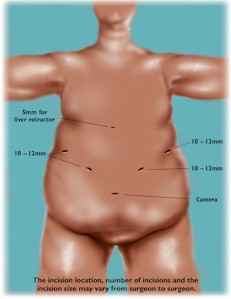
Weight loss surgery is done by laparoscopy also called minimally invasive surgery or keyhole surgery . It is a modern surgical technique in which operations in the abdomen are performed through small incisions (usually 2-3cm) as compared to larger incisions needed in traditional surgical procedures.
The abdomen is inflated creating sort of ‘air bubble’ as working space. Through 4 or 5 small incisions a camera and small instruments are placed inside your abdomen. The rest of the procedure takes place inside the abdomen.
After the surgery when a patient awakes he or she can experience pain in the shoulders due to the insufflation. Normally this pain disappears within a couple of days.
COMPLICATIONS
As with any surgery, there can be complications. This list can include:
• Deep vein thrombophlebitis 0.7%
• Non-fatal pulmonary embolus 0.5%
• Pneumonia 0.5%
• Acute respiratory distress syndrome 0.25%
• Splenectomy 0.9%
• Gastric leak and fistula 2.0%
• Duodenal leak 1.5%
• Distal Roux-en-Y leak 0.25%
• Postoperative bleeding 0.5%
• Duodenal stomal obstruction 0.75%
• Small bowel obstruction 2.0%
• Death 1.0%
DIET AFTER SURGERY
1. Adjusting eating behaviour
- Eat at diner table
- Have small meals and take your time,
- use 3 main meals and a few healthy snacks.
- Stop eating after first sensation of satiety,
- More bites can lead to vomiting.
- Drink slowly but not during a meal.
- Avoid alcohol,
- drinks containing sugar,
- sweets,
- cookies,
- chocolate.
- Avoid using pure sugar.
- Limit use of fat in meals.
Adaptation of eating after a Duodenal Switch goes in different steps from liquids to mixed to protein rich solid food. The meals are much smaller than normal and food needs to be much softer from texture. In every step it is important to drink enough water.
Step 1:
Liquid meals during first 14 days
Use:
- Low fat milk
- Low fat yoghurt
- Vegetable juices
- Soup (blended) or bouillon
- Protein drinks, etc
Step 2.
Slowly change to mixed foods by adding in the next 14 days
- mashed potatoes,
- cooked/mixed vegetables
- cooked fish, eggs
If this goes well then mixed meat, toasted bread and other food can be added, using small amounts. (= step 3)
Sleeve
INTRODUCTION
The Sleeve Gastrectomy is also called vertical gastroplasty, Gastric Reduction and even Vertical Gastroplasty It reduces the volume of the stomach by removing of a part of the stomach. Weight loss is generated by restricting the amount of food that can be eaten without any bypass of the intestines or malabsorption. Also the hungry feeling will diminish as the part of the stomach were these receptors are located will be removed. This procedure is done by laparoscopy. Because a part of the stomach will be removed this procedure is irreversible.!
PREPARATION TO THE PROCEDURE
When you are well informed and choose to have a ‘Sleeve-Gastrectomy’ then the following investigations have to take place:
1. Laboratory / Blood tests 2. Ultrasound of your abdomen 3. Electrocardiogram with cardiac check-up 4. Chest X-ray with pulmonary check-up 5. Gastroscopy 6. Consultation dietician
In case of regular medication usage one has to inform their surgeon, especially in case of blood thinners (aspirine, anti coagulants, anti-inflammatory drugs, http://www.ncpainmanagement.com/BloodThinners.htm ) as these need to be stopped before surgery.
On the day of surgery you will have to remain sober. If necessary some medication can be taken with a little water.
This procedure is not reversible !
PROCEDURE
With a Sleeve-gastrectomy a large part of the stomach is surgically removed by laparoscopy. This part is called ‘the greater curvature’ and is located on the left side of the stomach..
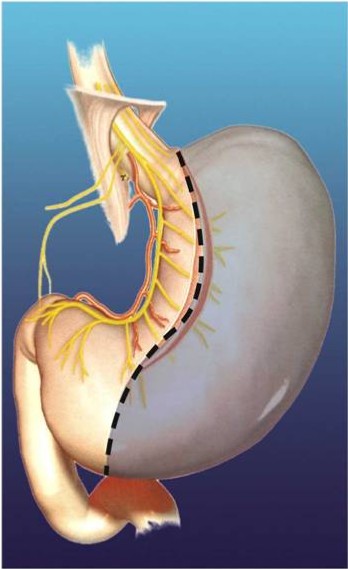
The stomach has normally the shape of a rugbt-ball but after surgery the shape is more like a banana. The exit of the stomach remains the same.
The volume after surgery is approximately 100 to 150 cc. It is a restrictive operation and can best be compared with the ‘Gastric Banding’.
SURGERY THROUGH LAPAROSCOPIE
Weight loss surgery is done by laparoscopy also called minimally invasive surgery or keyhole surgery . It is a modern surgical technique in which operations in the abdomen are performed through small incisions (usually 2-3cm) as compared to larger incisions needed in traditional surgical procedures.
The abdomen is inflated creating sort of ‘air bubble’ as working space. Through 4 or 5 small incisions a camera and small instruments are placed inside your abdomen. The rest of the procedure takes place inside the abdomen.
After the surgery when a patient awakes he or she can experience pain in the shoulders due to the insufflation. Normally this pain disappears within a couple of days.
COMPLICATIONS
1. During surgery or while hospitalized.
As with any surgery, there can be complications. These can occur during surgery, while hospitalized or after discharge. This list can include:
• Bleedings • Injury to the abdominal organs.
• Stomach ulcers or perforation.
• Deep vein thrombophlebitis with even non-fatal pulmonary embolus
• Gastrointestinal (sub)obstruction
• Urinary infection
• Woundinfection
• Pneumonia
• Heart attack
This list is not complete. There is even a very small risk of dying due to complications.
Special measures are taken to minimize the risk of complications. Complications which lengthen the hospitalisation are rare.
2. Late complications are very rare
DIET AFTER SURGERY
1. Adjusting eating behaviour
• Eat at diner table
• Have small meals and take your time, use 3 main meals and a few healthy snacks.
• Stop eating after first sensation of satiety, More bites can lead to vomiting.
• Drink slowly but not during a meal.
• Avoid alcohol, drinks containing sugar, sweets, cookies, chocolate.
• Avoid using pure sugar.
• Limit use of fat in meals.
Adaptation of eating after a Sleeve Gastrectomy goes in different steps from liquids to mixed to protein rich solid food. The meals are much smaller than normal and food needs to be much softer from texture. In every step it is important to drink enough water.
Step 1:
Liquid meals during first 14 days
Use:
• Low fat milk
• Low fat yoghurt
• Vegetable juices
• Soup (blended) or bouillon
• Proteindrinks, etc
Step 2.
Slowly change to mixed foods by adding in the next 14 days
• mashed potatoes,
• cooked/mixed vegetables
• cooked fish, eggs
If this goes well then mixed meat, toasted bread and other food can be added, using small amounts. (= step 3)
Redo-Surgery
Introduction
There are persons who have had weight loss surgery in the past. Some of them suffer from side effects or are not satisfied with the overall result. This can be because they lost to much weight or just to little.
Nowadays there are several new procedures which are an adaptation or a conversion of a previous procedure. Most of these procedures are offered at our Obesitycenter.
After Gastric Banding.
Some persons who had a gastric band experience insufficient weight loss, vomiting, pain or ‘slipping’ of the band or pouch dilation.
These patients can be offered several option. The band can be replaced by a Gastric Bypass or completely be removed. Normally this is done by laparoscopy.
After Vertical banded Gastroplasty / Mason
These persons often experience weight gain after many years or vomiting / nausea.
It is possible to convert this procedure to a Gastric Bypass. Normally this is done by laparoscopy.
After Biliopancreatic Diversion (BPD) or Scopinaro
This procedure was mostly performed in the ’80 – ’90. Some of these patients complain of diarrhoea, weight regaining and deficiencies.
It is possible to convert this ‘BPD’ or ‘Scopinaro’ into a Gastric Bypass. This is mostly done by laparotomy as there are frequent many adhesions.
We also developed a procedure where only an extra part of the stomach is removed. It is almost like a Sleeve Gastrectomy and helps again to loose weight. Advantage of this procedure is that it can be done by laparoscopy.
After Sleeve Gastrectomy
This procedure is often done as a first step of a two step procedure in extreme obese patients. After initial weight loss the second step can be either a Gastric Bypass or a Duodenal Switch procedure.
Also a re-Sleeve gains a lot of popularity among those patients.
Normally these procedures are done by laparoscopy.
After Gastric Bypass
A small group of patients can eat again a lot after a Gastric Bypass and gain some weight. For this small group there is now a new procedure where a silastic ring is added to the Gastric Bypass.



 Inschrijven voor Kinesitherapie
Inschrijven voor Kinesitherapie